Bladder Blood Flow as a Regulator of Bladder Function
Nearly half of all diabetic patients experience lower urinary tract symptoms (LUTS), which significantly reduce their quality of life. Although ample evidence links impaired bladder blood flow to LUTS, a fundamental gap exists in our understanding of bladder blood flow regulation and its effects on bladder function.
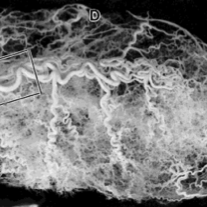
The urinary bladder is highly vascularized, with unique properties that maintain vessels in a state of maximal dilation to maintain tissue perfusion during bladder distention and filling. While bladder blood flow decreases as the bladder fills, it also markedly increases immediately following voiding. How bladder vascular tone is regulated, however, is largely unknown.

We discovered that isolated, pressurized bladder arterioles do not develop pressure-induced constriction (“myogenic tone”), but do respond to multiple vasoactive compounds, including those produced by the urothelium. Interestingly, we found that blockade or knockout of inward-rectifier K+(KIR2.1) channels causes constriction and development of pressure-induced myogenic tone, suggesting that this channel provides a unique mechanism for opposing myogenic tone. (Links to our paper can be found in our Publications.)

The goals of this project are to understand how urinary bladder vascular function affects micturition, and how the unique properties of the bladder vasculature contribute to this regulation in normal health and diabetes. We postulate that decreased blood flow, caused by increased vascular reactivity, leads to bladder dysfunction in diabetes.